Monday 15 July 2013
Saturday 13 July 2013
Don't Call Me Crazy Review
BBC3 fired the mad world season into action with a shocking, yet truthful insight into life in an adolescent psychiatric unit, filmed in one of the largest units of its kind - the McGuinness unit in Manchester. They showed a wide range of mental illnesses including depression, anxiety disorders and psychotic episodes with a balance between the voluntary and sectioned patients. The overall aim of the documentary was to raise awareness and break down the stigma of mental illness by educating people on the facts of what life is like for young people experiencing such problems.
One successful quality was the portrayal of both good and bad times witnessed by the millions of viewers, showing real honesty of life in a psychiatric unit. The raw emotions expressed by the patients touched viewers in many ways but most importantly they showed the ongoing struggle with twisting emotions and heightened mood swings resulting in unpredicted behaviour and responses. However, the BBC have been criticised for showing such extreme emotions and it has been argued that the programme was extremely triggering for those who have past histories of mental illness and those presently suffering. Every episode addressed the issue of self-harm and although this tackled many myths and settled the fact it is used as a coping mechanism and not suicide, it was still considered to be distressing for may individuals. Not only was the subject discussed, almost all of the teens' cuts were recorded, showing arms full of deep cuts and scratches. While setting the record straight about the self-destructive coping mechanism, thousands of young people found this triggering leading to recovered people resorting to the same behaviours - leading to physical and psychological harm- something that the BBC chose to ignore. This was also the case with eating disorders, as a patient was repeatedly filmed whilst dramatically struggling with anxiety and later was shown to be recording the amount of hours managed without food. This in turn was argued to be triggering, causing psychological harm to viewers. On the other hand, the debate about truth vs triggering was probably considered by broadcasters leading to what they perceive as the most sensible decision. In addition, it was stated that there are 11 beds for females and only 4 for males in the unit. This was, however, legitimated by a professional explaining that females can talk more easily about their problems while on the other hand, the males tend to keep their emotions bottled up. This generalisation that is made may not be accurate for all hospitals therefore not making a valid statement.
Another important misconception about psychiatric units was dealt with my the clinical psychologist who explained that young people do not leave the ward completely cured and that the aim is to help and provide coping strategies for the teenagers so they are then able to cope better when they are alone in the outside world. The staff filmed provided an illuminating insight as to what life in the unit is like for them and their responsibilities. This was exceptionally interesting and brought many jobs into the light that people many have not considered or known much about. Review groups enabled the viewers to see the stages in which professionals go through when treating mentally ill patients. Others clips showed art therapy, physical therapy and tasks carried out by the occupational therapist which portrayed many of the recovery therapies that most patients go through.
One particular patient was filmed experiencing what appeared to be psychotic episodes. While searching for a clear diagnosis, it was found that the 14 year old girl having hallucinations and delusions were actually ways of coping with the abuse she had experienced in childhood. Although she had been adopted, she explained that she has younger siblings still living with the parents who are obviously abusive. This brought to light a worryingly dangerous situation which the BBC failed to commentate on.
Despite these few criticisms, the episodes succeeded in portraying the honest reality of millions of teenagers and the 3,500 that walk through the hospital ward every year. It challenged the stereotypical views about mental illness and addressed how the young people feel judged when they are in the outside world. Mental illness is no less serious than physical illness, and with the continuation of programmes such as Don't Call Me Crazy, more and more people can become more open minded to the reality of so many lives. The fact that so many people are completely shocked about what they viewed in the documentary proves the long silence of mental illness...
Do you still judge mental illness?
Wednesday 10 July 2013
Don't Call Me Crazy
BBC Three's Don't Call Me Crazy gives a very truthful yet sensitive insight into an adolescent psychiatric unit, reflecting the reality of life for the patients, as well as highlighting each of the jobs performed by staff. It shows the reality of over half a million young people in Britain who have to deal with mental illnesses. 3,500 people pass through the doors of the Mcguinness Unit in Manchester each year.



http://www.bbc.co.uk/iplayer/episode/p01b871m/Dont_Call_Me_Crazy_Episode_1/
http://www.bbc.co.uk/iplayer/episode/b036qjt5/Dont_Call_Me_Crazy_Episode_3/
Can be triggering for some- self harm, depression, eating disorders.
Twitter:
#dontcallmecrazy
@mindcharity
@TimeToChange
@bbcthree
@CherieGoddard
Beth's Experience
Beth has suffered from depression and eating disorders since she was 14. She stayed in the McGuinness Unit for six months.

Depression
Just take a few seconds to picture this in your mind; you’re standing inside a tall dark room and no matter how hard you try you just can’t get the lights to switch on. You see figures but all you can think of is that they are going to hurt you, leave you or just reject you. Instead of getting to know these figures and coming up with a plan to get out of the black hole, you just push them away in fear of them getting to know the real you. Just imagine putting up with that for months… even years. Well this is similar to what depression can feel like; it’s a long lonely battle. This is why many people keep quiet about their mental health issues because of the fear they might get judged, it’s not a physical health problem that you can see but it doesn’t mean they aren’t real.
Life in the unit
My stay at the McGuiness Unit was very long and hard; I find it hard recording the first few weeks/months, that’s just because of how bad my depression had got. Some days it was like a never ending nightmare that I couldn’t awake from, whereas others I have kept as memories. During my hospitalisation I made some great friends… all still ordinary people like myself that have just reached a little blip in their lives. Soon enough friends become family in a closed environment, there would always be somebody there to talk to and confide in when you don’t want to talk to staff. However there is one goal which everybody strives for and that is to be discharged. I saw some patients come and go within a week, whereas others were in there the whole 6 months I was, these are the people I miss the most.
Dancing again
Since leaving the unit on April 2nd I have tried to get back to normality. I have gone back to dance, which just recently I won the British isle championships. Dance means a lot to me, I’ve done it since being tiny and when I first got ill with my eating disorder I had to give it up because my body just couldn’t cope with the stresses I was putting it under. This is my biggest achievement of all; being able to dance again. I have missed too much college to be able to go back this year but my plans are to return and finish my second year in September, then off to university I go. Other than that, and the holiday I am going on with my friends. I don’t really have many plans for the future except for keeping myself well.
Stigma
The stigma around mental health is terrible, the words ‘mental health’ does not mean ‘crazy’, one in four people suffer from a mental health illness, that means somebody in your family, your next door neighbour or even a best friend could be suffering. It is important that they seek help as many people can lose their lives through mental illnesses; I know I nearly did, and this is why I want to spread the awareness and stop this disease from damaging any more people. Eating disorders have the highest mortality rate of any mental illness… it’s not a laughing joke now is it? Just because somebody isn’t walking around with a cast on their leg, doesn’t mean they aren’t suffering. Mental illnesses are far more complex and severe than just a broken leg.
Just because you can’t see it doesn’t mean it isn’t there.
Dr Andy Rogers
Dr Andy Rogers is the Head of Psychological therapies at the McGuinness unit, he discusses the benefit of the unit for his young patients.

What does the McGuinness unit offer?
The McGuinness unit is a specialist Adolescent Inpatient ward for young people aged 13 to 18 who require assessment and treatment for a range of complex mental health difficulties including severe mental illness. The service provides day-to-day therapeutic care, as well as education, in a safe and nurturing environment.
For many young people who experience mental health difficulties, the support of those that they know and trust is extremely important in their recovery. Most young people, who experience mental health difficulties will be referred by their GP to specialist Child and Adolescent Mental Health Services (CAMHS). CAMHS, aided by family and school will support the recovery of the young person at home and in the community.
However, for some young people, their distress is so severe and the difficulties they encounter are so complex that they become extremely vulnerable in the community.
At times a young person may feel very unsafe and be at risk of harming themselves or others. Some young people in these circumstances may have received a diagnosis, which is a way of helping them and others to understand their experiences and can give a guide as to what treatment may help their recovery. Young people who come to the McGuinness Unit may have one or more diagnoses such as: anxiety, depression, psychosis, bi-polar disorder, eating disorder or post-traumatic stress disorder. The Young People may also present with distress that leads them to harm themselves (self-harm) or display other concerning behaviours such as aggression, excessive washing or repeated checking.
Many young people do not have a diagnosis at the time of their admission, but often their distress and behaviour is very concerning for them and other people. These young people need to spend some time at the McGuinness Unit so that their difficulties and needs can be assessed and a plan of support and treatment developed.
The McGuinness Unit is an ‘open’ unit, in that the majority of the young people recognise they need support and come to us voluntarily. For a small number of young people who are particularly distressed and are struggling to accept that they require help, there may be a need for them to be kept in hospital against their wishes and prevented from leaving. . This means a young person is detained under a legal order under the Mental Health Act, a ‘Section’. This allows for a young person remain in hospital for a sufficient period of time, to either assess or treat their mental health difficulty. Detention under the Mental Health Act is undertaken with the consent of the young person’s parents or nearest relative.
Who works at the unit?
Our Clinical Team is made up of people from a variety of professional backgrounds including Psychiatrists, Clinical Psychologists, Nurses, Occupational Therapists, Social workers, Arts and Psychological Therapists, Teachers and Dieticians. We also include our Domestic staff, administration staff and management as part of the team!
In order to support young people in their recovery, we provide a range of interventions for them and their families including: building positive relationships with staff and other young people, engaging them in fun activities, education and sport, supporting them in daily living skills such as cooking, budgeting and shopping, and more formal psychological therapies such as cognitive-behavioural therapy, family therapy and art and music therapy. These may be delivered individually or in a group. While medication is used to treat some illness in young people, it is often not the first line of treatment, and when used, is always supplemented by these other interventions. We also have an onsite education provision ‘Cloughside College’ that provides formal education tailored to the needs of the young people in our care.
Some of the guiding principles of the McGuinness unit highlight that the young people we work with are not ‘mini-adults’, are still learning and developing and are able to achieve recovery. As such, the young people we work with are treated as typical adolescents, who happen to experience mental health difficulties, often as a result of their coping resources not being fully developed or having become overwhelmed. We also believe that Young People should spend as short a time as necessary in hospital. This means that right from the start of their time with us, they are supported in a developmentally appropriate way to return to challenges and rewards of their daily lives as quickly as possible. This involves helping young people to build their coping skills, confidence and resilience, improve relationships with those in their lives that can support them and build a lasting plan for the future. If we can help to achieve this, we hope to significantly reduce future distress, increase the chance of the young people being able to manage the ups and downs life more effectively and ultimately have a positive and productive future.
Vicki Ray
Vicki Ray is an occupational therapist, who works with the teenagers at the McGuinness Unit.

Occupational Therapy
My role as the Occupational Therapist (OT) is to look at how the young person’s illness affects them on a day to day basis. When young people are admitted to the ward, I introduce myself and explain what my role is all about. Many young people have not worked with an OT before and it is important for them to understand how I may be able to help them as part of their treatment and begin to build a therapeutic relationship with them.
When in the unit, the young person is given time to speak to nurses and doctors about their condition but with me, I try and find out more about that individual such as their hobbies, interests, likes and dislikes and what makes them tick. I aim to find out how the experience of the illness affects the young person.
Throughout the occupational therapy sessions I aim to help change the way the young person sees the outside world and how they fit within the world and that it’s not necessarily a big, bad, scary place. It’s all about getting to know the young person as an individual.
I explore how the young person’s illness may be affecting their daily routine. Their illness can often affect how they manage on a day to day basis completing everyday tasks, which can include managing a routine with school/college, seeing friends/family, engaging with the community and social activities such as using public transport. By attending the family home I can gain feedback from the family and see how the young person copes at home.
The Road to Recovery
Use of activities is an important part of the young person’s road to recovery. By getting to know the individual I can incorporate their hobbies into activities which they will do on the ward. By focusing on a task, this will often distract the young person from the negative feelings or symptoms of their illness.
Activities can often involve art work, board games and console games. By monitoring the activity sessions, we can assess how the young person is coping by looking at ability to follow instructions and concentration span of the young person. This helps us learn more about that individual and how we can tailor activities further to help them recover.
When a patient is admitted their general mood is low and they can often feel isolated. By using different activities involving something of meaning to the young person this can help them feel more positive. I would tailor the activities to suit the needs of the young person. Throughout this process I will talk with the young person and help them recognise their anxious feelings and how to deal with them.
On reflection of the activity the young person will often realise that the task was not scary or difficult which will result in anxiety levels decreasing and confidence levels increasing. By the time the young person leaves the unit their confidence levels have increased, they are more sociable and will initiate conversation more. It’s all about challenging some of those anxious thoughts the young person has and changing the way they think about certain situations they may feel are scary.
A large part of my role is facilitating, with other therapists, a range of therapeutic groups for young people. We offer a wide range of groups outside of the academic term including a recovery group, meal preparation groups, baking, social groups, health promotion, current affairs and art based groups. These groups are encouraged as positive social activity can help aid recovery.
Pete Croft
Pete Croft is a Mental Health Nurse at the McGuinness Unit, he talks about his experiences.
No two days the same
I’ve been a Registered Mental Health Nurse at the McGuiness Unit for four years now and I’ve never had two days that are the same. When patients come through those doors you have to be open-minded and ready for anything that might come your way.
When a new patient arrives they can be extremely frightened with the idea of arriving in this strange place, so part of my role is to ensure that they have an easy introduction to the unit and try and make it seem less like a place they’ve been forced to come to. I like to think that this helps them settle in; despite the fact they may be distressed or troubled due to their mental health.
After showing patients and their families around the building, my focus is to complete the admission process. I will ask a doctor to undertake a physical examination, provide patients with details of their stay, such as what to expect when being a patient here, when they have their one to one session and who their named nurse is. Once they’ve settled in, I have to make sure all the clinical admission paperwork associated with a new patient, such as liaising with the pharmacy for medication, mental state exams and Mental Health Act paperwork is done. The paperwork side of things can be very time consuming, but it’s needed to complete a comprehensive assessment for each patient.
The nursing support and care I provide to the patients whilst they are at the McGuiness Unit varies every day and that’s what makes it interesting. I can be spending time with a young person, discussing their inner most thoughts and concerns and helping them to develop some resilience and coping strategies, then the next minute I can be managing the aftermath of a serious incident where a young person needs support to manage their emotions. Once that is dealt with I can be organising activities for patients in conjunction with the Occupational Therapy Team or attending reviews to discuss progress of individual patients. It changes minute-by-minute and can be a challenging, but it really is a rewarding job.
Vulnerable patients
Being there for the patients who at times are very vulnerable, supporting them when they may feel distressed and can harm themselves or others is a big part of what we do here. These situations can be quite tense but the most important part of this role is being there for someone when things aren’t going well. We have a number of people who self-harm and dressing their wounds has become a part of my role that isn’t something I enjoy, but I know that the effort I make after the event with that patient is something they need. The worst thing would be to just be negative with the young person and not allow them to talk about their problems that have led to them self-harming.
A lot of the people who come through here find a real comfort in someone just simply lending them an ear and allowing them to talk about their issues. As a nurse, something as simple as talking and being a friendly face can help develop a flicker of hope that their situation can get better. When you see those young people you’ve helped making progress it’s something that makes you come back into work each day.
In the documentary you can see me trying to lift the spirits of one of our service users with a bit of humour, and through simply telling a joke (albeit a bad one!) you can change that person’s perception of how their day is going or how well their treatment is progressing. I know that the time I take to listen to their concerns, or chat to them about daily life in the unit can really make a difference.
Being a Mental Health Nurse
Working in Mental Health and being a registered nurse wasn’t actually my first career choice… before this I was a policeman for Greater Manchester Police for a couple of years. There are aspects of both jobs that are similar, especially when you have to deal with confrontation. The unit has a number of people who suffer from mental health issues that could lead them to act aggressively towards other service users or patients, and part of my role is to ensure that those instances don’t escalate. I’m sure that if you asked some of the young people in the unit they would probably say that we are trying to control them, but the reality is I’m there to protect their welfare whilst they receive care, and although that does mean having to restrain people or be authoritative at times, it is only done with their best interests at heart.
Being a mental Health Nurse isn’t a job you get into for the money, you do it so you can help people get better, and seeing the progress young people make from when they come in to when they leave, whatever length of time that is, makes you proud of what you’ve done to help them. The job can be stressful, but at the same time the reward of helping someone who hasn’t really begun their life and getting them back on track is what we’re all here for.
http://www.bbc.co.uk/iplayer/episode/p01b871m/Dont_Call_Me_Crazy_Episode_1/
http://www.bbc.co.uk/iplayer/episode/b036qjt5/Dont_Call_Me_Crazy_Episode_3/
Can be triggering for some- self harm, depression, eating disorders.
Twitter:
#dontcallmecrazy
@mindcharity
@TimeToChange
@bbcthree
@CherieGoddard
WOAH
Amazed to see how many page views my poor, abandoned blog has from 10 different countries!

Thank You!
Friday 5 April 2013
Friday 15 March 2013
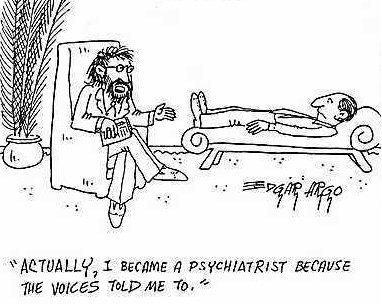
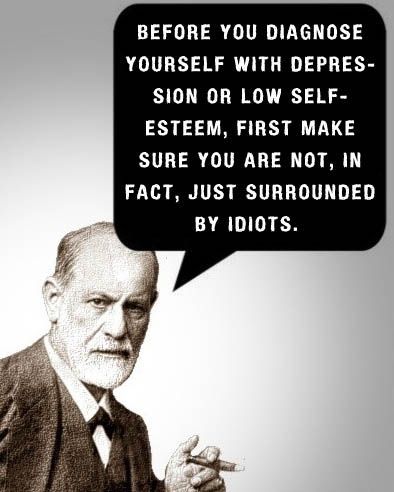
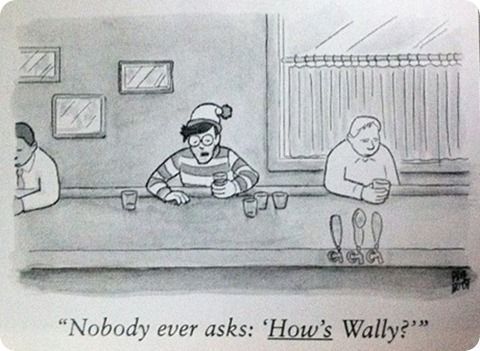
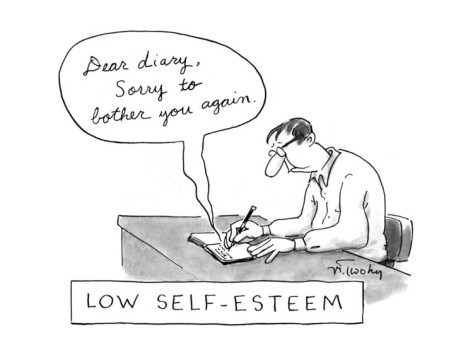
These just have to be blogged!
Thursday 14 March 2013
POSITIVE PSYCHOLOGY
Positive psychologists seek to 'find and nurture genius and talent' and to make 'normal life more fulfilling', rather than merely treating mental illness.
Examples
Dyslexia definition-
Dyslexia is a very broad term defining a learning disability that impairs a person's fluency or comprehension accuracy in being able to read, and which can manifest itself as a difficulty with phonological awareness, phonological decoding, processing speed, orthographic coding, auditory short-term memory, language skills/verbal comprehension, and/or rapid naming.
This definition contains the elements of the condition that are the individual's weaknesses. This can have a long term, dramatic effect on a child and they can carry feelings of inadequacy around with them for the rest of their lives. Rather than concentrating on the negatives, positive psychologists believe that you should always focus on the individual's strengths. Instead of dwelling on the negatives, encouragement of the person's strengths is required for their self esteem. For example, Dyslexics often have many of these qualities:
- Perception: the ability to alter and create perceptions;
- Highly aware of the environment;
- Highly curious;
- Great intuition and insightful;
- Thinking and perceiving multi-dimensionally (using all the senses);
- A lively imagination;
- Can experience thought as reality;
- Creativity;
- Easy adoption of change;
- Holistic, see the big picture, don’t get lost in details, get to the important aspects;
- See patterns, connections, and similarities very easy;
- Concentration;
- Can be very driven, ambitious and persistent;
- Superior reasoning;
- Capable of seeing things differently than others;
- Love for complexity;
- Simultaneous multiple thought processing;
- Not following the crowd;
- The ability of visual, spatial and lateral thinking.
and go on to work in areas such as:
- Science/research
- Psychology
- Teaching
- Manager in people-relate occupations
- Businesspeople in general
- Marketing and sales
- Interior/Garden/mode design
- Culinary arts
- Woodworking
- Carpentry
- Artiste
- Painter/sculptor
- Actor
- Graphic art
- Architecture
- Designer
- Mechanics
- Engineering
- Photography
- Music
- Athletics
- Computing
- Software design
- Electronics
Another short example is to not make people suffering from depression less depressed in treatment, but to help them find something to make them happy.
Monday 4 March 2013
Friday 1 March 2013
Sunday 24 February 2013
Monday 18 February 2013
ALL RODILLIAN TEACHERS MUST READ THIS!
CLASSROOM PHOBIA/ANXIETY
SYMPTOMS TEACHERS SHOULD EXPECT PUPILS TO DISPLAY AND THE MAIN WARNING SIGNS:

SYMPTOMS TEACHERS SHOULD EXPECT PUPILS TO DISPLAY AND THE MAIN WARNING SIGNS:
- Extreme quietness
- Unable to initiate conversations
- Lack of eye contact
- Often refuses to do things
- Doesn't join in
- Won't speak at all
- Fear of public speaking
- Fear of the unknown
- Fear of being judged (happens loads)
- Won't be able to think on the spot e.g. will say they don't know the answer due to not being able to think of it quick enough/ they will be too worried to think about it at all- often occurs in problem solving (maths) or offering their own opinion or interpretation (English lang and lit)
- Stutters
- Sighs
- Disinterested in lessons
- Irritability and fidgeting
- Dread of events in the future
- Looks worried/anxious
- Looks exhausted
- Drinks lots
- Leaves to go to the toilet (anxiety causes frequent urination/ maybe just escaping the situation)
- Will talk about anything other than work- suggests lack of confidence in work- some won't actually know the answers due to not listening as they are preoccupied with other thoughts and feelings. The more they try to listen the more they won't be able to.
- Frequently absent
- Abrupt with teachers
- Uses physical illness as an excuse for the real problem
- May even cause panic attacks- read The Panic Cycle Post.
May often coincide with other disorders such as Social Anxiety, Generalised Anxiety Disorder and depression. Often the cause of selective Mutism.
The problem is slowly becoming more recognised by teachers.....
Teachers have the power to create a safe and comfortable classroom environment where pupils accept the teachers control as a result of being able to trust the way they conduct lessons.

Skinner- Operant Conditioning
Reinforcement
Skinner showed how positive reinforcement worked by placing a hungry rat in his Skinner box. The box contained a lever in the side and as the rat moved about the box it would accidentally knock the lever. Immediately it did so a food pellet would drop into a container next to the lever. The rats quickly learned to go straight to the lever after a few times of being put in the box. The consequence of receiving food if they pressed the lever ensured that they would repeat the action again and again.
Positive reinforcement strengthens a behavior by providing a consequence an individual finds rewarding. For example, if your teacher gives you £5 each time you complete your homework (i.e. a reward) you are more likely to repeat this behavior in the future, thus strengthening the behavior of completing your homework.
Skinner showed how negative reinforcement worked by placing a rat in his Skinner box and then subjecting it to an unpleasant electric current which caused it some discomfort. As the rat moved about the box it would accidentally knock the lever. Immediately it did so the electric current would be switched off. The rats quickly learned to go straight to the lever after a few times of being put in the box. The consequence of escaping the electric current ensured that they would repeat the action again and again.
Sunday 17 February 2013
Dissociative Personality Disorder
Dissociative Personality Disorder
DSM-IV-TR criteria- Longstanding or recurring feelings of being detached from one’s mental processes or body, as if one is observing them from the outside or in a dream.
- Reality testing is unimpaired during depersonalisation
- Depersonalisation causes significant difficulties or distress at work, or social and other important areas of life functioning.
- Depersonalisation does not only occur while the individual is experiencing another mental disorder, and is not associated with substance use or a medical illness.
The DSM-IV-TR specifically recognises three possible additional features of depersonalisation disorder:
- Derealisation, experiencing the external world as strange or unreal.
- Macropsia or micropsia, an alteration in the perception of object size or shape.
- A sense that other people seem unfamiliar or mechanical.


The media and mental health medication article
‘Hooked on happy pills’? How the media demonises mental health medication
Language is very telling of attitudes - would it be the same talking about medication for
high blood pressure?
high blood pressure?
http://www.independent.co.uk/voices/comment/hooked-on-happy-pills-how-the-media-demonises-mental-health-medication-8494801.html
Saturday 16 February 2013
LOST CHILDREN- C4
Josh
Shows the the effect of having a drug-addict mother, alongside the effects being put into care and moved between 24 foster placements can have on a child.
With intimate access to staff, pupils and families, this film tells the surprising and touching story of one of the High Close School's most challenging children: Josh. Filmed over a year, the programme follows the ups and downs of his education and explores his history to discover what made him the way he is.
Courtney
Shows ADHD and the possible causes for this illness to develop from situational events from the past.
Twelve-year-old Courtney from Liverpool has been diagnosed with ADHD, and was excluded from her primary school for disruptive behaviour.
Shows the the effect of having a drug-addict mother, alongside the effects being put into care and moved between 24 foster placements can have on a child.
With intimate access to staff, pupils and families, this film tells the surprising and touching story of one of the High Close School's most challenging children: Josh. Filmed over a year, the programme follows the ups and downs of his education and explores his history to discover what made him the way he is.
Fourteen-year-old Josh is the school's tough man. He was taken away from his heroin-addicted mum and put into care at the age of three. He had a staggering 24 moves between foster placements before the age of six, together with his younger sister Demi.
However, for the past eight years, Josh and Demi have lived with their adoptive mother, former social worker Sue, who is determined to provide them with a loving and stable home.
'You think a lot of love and lot of attention will be enough,' Sue says. But soon Josh's angry outbursts and aggressive behaviour mean that both Sue and the teachers at High Close are struggling to help him.
As the story of Josh's past unfolds, tensions escalate at school, and he brings his mother closer to breaking point. Can Josh avoid repeating the mistakes of his birth family and make the necessary changes to remain at High Close?
http://www.channel4.com/programmes/lost-children/4od#3407684Courtney
Shows ADHD and the possible causes for this illness to develop from situational events from the past.
Twelve-year-old Courtney from Liverpool has been diagnosed with ADHD, and was excluded from her primary school for disruptive behaviour.
She's now starting her second year as a boarder at High Close School in Berkshire, which is run by Barnardo's and is home to some of Britain's most troubled children.
According to Nikita, Courtney's key worker, she has tremendous potential. But as Courtney approaches her teenage years her behaviour is deteriorating fast.
Struggling to find words for how she feels, Courtney says it's like there's 'a little cell in inside my head that says "don't care". It's like my head's changed.'
Behind Courtney's anger there's an extraordinary family story that stretches back more than four generations, from her mother, Sara, to her great-grandmother, Edna.
Loving and close, these four generations are a remarkable testimony to the strength of their family ties but they're also players in a story of troubled and sometimes violent relationships.
Through the years, the women in the family have turned to each other for support. But despite their love for each other, events in their lives seem to keep on repeating themselves.
As Courtney's mother Sara inches closer to breaking point, Jonathan Newport, the dedicated deputy head teacher of High Close, is running out of ideas.
Courtney's on the brink of exclusion at an extremely understanding school, and keyworker Nikita is worried if she leaves there she will 'fall through the net'.
With the help of her family and teachers, can Courtney turn her life around?
Thursday 14 February 2013
Cane Hill, London
Cane Hill was an insane asylum in Croydon, London in use until 1991 when – by all appearances – everyone just got up and walked out. Some of the inmates were transferred to other secure locations but the hospital, and much of the medical apparatus still remains.
Friday 8 February 2013
Teenage drinking and mental health.
Teenagers who drink heavily are also more likely than their peers to have behavioral problems or symptoms of depression and anxiety, a new study finds.
The study of nearly 9,000 Norwegian teenagers found that those who said they had been drunk more than 10 times in their lives were more likely to have attention and conduct problems in school. Meanwhile, heavy-drinking girls showed higher rates of depression and anxiety symptoms.
The findings, published in the online journal Child and Adolescent Psychiatry and mental health, are based on a one-time survey. They do not, therefore, show whether the drinking came before or after the teenagers' other problems.
That said, conduct and attention problems do tend to develop early in childhood, and would be less likely to arise in adolescence, Strandheim told Reuters Health.
But regardless whether drinking or other problems comes first, the bottom line is that parents should be aware that they often go hand-in-hand, according to the researcher.
The findings are based on a survey of 8,983 13-to-19 year olds. 80 percent said they had tried drinking, when 57 percent had gotten drunk at least once.
Similarly, 35 percent of teenagers who acknowledged conduct problems- getting into fights or clashes with teachers- also admitted to getting drunk frequently. That compared roughly to 27 percent of teens with few conduct problems.
Anxiety and depression symptoms were also linked to more frequent drinking binges, but only among girls.
It is important to intervene early to keep all teenagers from abusing alcohol, Strandheim stressed. however, the researcher said, it may be particularly important to girls with signs of depression or anxiety, and teen with attention problems or behaviour issues.
SOURCE: Child and Adolescent Psychiatry and Mental Health
Thursday 7 February 2013
DANCE THERAPY
Dance/Movement Therapy
Dance/movement therapy, or dance therapy is the psycho therapeutic use of movement and dance for emotional, cognitive, social, behavioral and physical conditions. As a form of expressive therapy, DMT is founded on the basis that movement and emotion are directly related. The ultimate purpose of DMT is to find a healthy balance and sense of wholeness.
Since its birth in the 1940s, DMT has gained much popularity and has been taken to more serious and beneficial levels. Over the years, the practices of DMT have progressed, however, the main principles that founded this form of therapy have remained the same. Influenced by the “main principles” of this therapy, most DMT sessions are configured around four main stages: preparation, incubation, illumination, and evaluation. Organizations such as the American Dance Therapy Association and the Association for Dance Movement Therapy, United Kingdom maintain the high standards of profession and education throughout the field. DMT is practiced in places such as mental health rehabilitation centers, medical and educational settings, nursing homes, day care facilities, and other health promotion programs. This form of therapy which is taught in a wide array of locations goes farther than just centering the body. Specialized treatments of DMT can help cure and aid many types of diseases and disabilities. Other common names for DMT include: movement psychotherapy and dance therapy.

The theory of DMT is based upon the idea that “the body and mind are inseparable”.
“Dance movement therapy rests on certain theoretical principles. These are:
- Body and mind interact, so that a change in movement will affect total functioning
- Movement reflects personality
- The therapeutic relationship is mediated at least to some extent non-verbally, for
- example through the therapist mirroring the client’s movement
- Movement contains a symbolic function and as such can be evidence of unconscious process
- Movement improvisation allows the client to experiment with new ways of being
- DMT allows for the recapitulation of early object relationships by virtue of the largely non-verbal mediation of the latter”
Through the unity of the body, mind, and spirit, DMT provides a sense of wholeness to all individuals.
The Creative Process
The creative process has four stages, which occur during DMT. Each stage contains a smaller set of goals which correlate to the larger purpose of DMT. The stages and goals of DMT vary with each individual. Although the stages are progressive, the stages are usually revisited several times throughout the entire DMT process. The four stages are:
- Preparation: the warm-up stage, safety is established
- Incubation: relaxed, let go of conscious control, movements become symbolic
- Illumination: meanings become apparent, can have positive and negative effects
- Evaluation: discuss significance of the process, prepare to end therapy

- DMT can be used to heal serious disorders and diseases. Although DMT is promoted to reduce stress and center the body, this therapy is very effective in helping to heal other disabilities and diseases. Examples of these include:
- Autism: therapists connect on a sensory-motor level, provides a sense of acceptance and expands skills and cognitive abilities, increases maturity
- Learning Disabilities: develops better organizational skills, learns/experiences control and choice, higher self confidence, new inspirations to learn
- Mental Retardation: improves body image, social skills, coordination, and motor skills, promotes communication
- Deaf and Hearing Impaired: reduces feelings of isolation, provides inspiration for relationships
- Blind and Visually Impaired: improves body image, motor skills, and personal awareness
- Physically Handicapped: improves motor skills and body image, provides a way to communicate and express emotions
- Elderly: provides social interaction, expression, and exercise, alleviates fears of loneliness and isolation
- Eating Disorders: alters distorted body images which helps end destructive behaviors, discovers symbolic meanings behind disorder/food
- PTSD: weaves together past and present through symbolism in a “safe place” to confront painful memories
- Parkinson's Disease: uses rhythm to help reduce body dysfunctions which improves motor abilities, balance, and use of limbs
- Holistic Birth Preparation: implores relaxation techniques to reduce anxiety, learn breathing techniques and release energy, builds confidence to help cope with labor, birth and early parenting
- Dementia: improvement in articulacy, oral and body language communication and increased pleasure/enjoyment of activities as well as an increase in involvement of activities
- Depression: reduces stress, anxiety, number of visits to the doctor, medication intake; help build and strengthen bonds and relationships
Abnormality
What is madness?
Can abnormality really be defined?
Abnormality definitions
1. Failure to function adequately.
2. Deviation from social norms.
3. Deviation from ideal mental health
Tuesday 5 February 2013
ORPHAN
American psychological thriller. Kate and John, a couple with 2 children decide to adopt a nine year old Russian girl, after their third child was a still born. Kate, who is recovering from alcoholism, soon discovers that there is something not quite right about Esther. Esther soon forces Max, Kate and John's deaf-mute daughter into her dangerous and disturbing plots.... as the family begins to deteriorate as a result of her distressing and evil personality and John's blindness to see what she is really doing..... Will you spot Esther's secret?


Presents family relationships, adoption, attachments, alcoholism and mental illness.
Monday 4 February 2013
Schizophrenia simulations
Schizophrenic's experience all different types of positive symptoms(addition to normal behaviour) There are no exact same voices heard by all - these are just a few cases (and obviously may not be accurate)
Subscribe to:
Posts (Atom)







.jpg)




.jpg)